Often, as the result of media reportage, we develop the impression that increasing our intake of a single food or nutrient is the key to a healthy diet.
In fact, the three dietary practices for which there is the most scientific support with respect to benefit to human health are increased intake of vegetables and fruit, management of glycemic load (the impact of the foods we eat on blood-sugar levels) and maintenance of a healthy body-weight.
Considered in this light, the relationship between the standard North American diet (i.e., over-size portions and high in red meats, refined grains and “junk” foods) and chronic disease becomes clear.
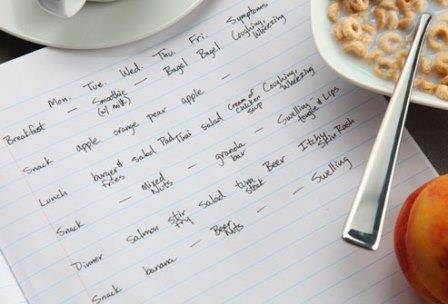
It is possible to eat a healthy, balanced diet, consistent with what the Harvard School of Public Health describes a “Prudent Diet”, by eating according to the following simple guidelines at each of your three daily major meals (breakfast, lunch, dinner).
Two handfuls of “non-starchy” vegetables and/or fruits:
- “Starchy” vegetables include potatoes, sweet potatoes, yams, squash, turnips, parsnips and beets
- Two colours of fruits and/or vegetables at each meal
- Fruit servings should be limited to three daily
Palm-sized serving of “starches”:
- Including “starchy” vegetables, grains and grain products (breads, pastas)
- Emphasis should be on whole grains and grain products
Palm-sized serving of protein source:
- Including fish, meats, eggs, dairy products, tofu products, beans, legumes, and nuts and seeds
- For non-vegetarians, fish should be eaten two to five meals weekly
- “Red” meats (including pork) should be limited to two meals weekly
Benefits of a Balanced Diet Compared to a Standard North American Diet
- Less calories
- Less saturated fats
- Less refined carbohydrates
- More fiber
- More vitamins and minerals
- Better blood-sugar control
Posted: 2015 March 12
References
Burford-Mason A. Nutrition for Docs 2008; 2008 Oct 4-5; Toronto, ON: Ontario Society of Physicians for Complementary Medicine and The Complementary Medicine Section, Ontario Medical Association; 2008.